It is a liquid connective tissue which circulates in closed
vascular system through out the body which supply nutrition oxygen to the
tissue and also remove the metabolic
waste products.
Definition
It may be defined a special connective tissue in which there is a
liquid part which is know as plasma and formed elements R. B.Cs. W.B.C. ,
platelets which are present in plasma.
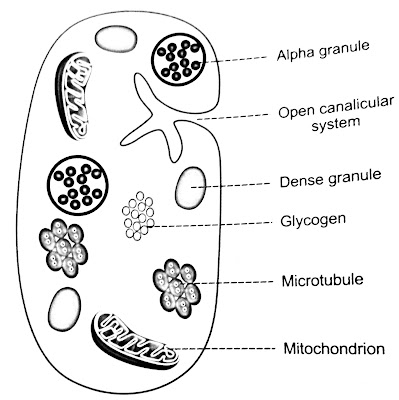
Platelets or thrombocytes are the formed of blood. Platelets are
small colorless non nucleated and moderately refractive bodies.
FUNCTIONS OF PLATELETS
1. ROLE IN BLOOD CLOTING
2. ROLE IN CLOT RETRACTION
3. ROLE IN PREVENTION OF BLOOD LOSS
4. ROLE IN REPAIR OF RUPTURED BLOOD VESSEL
5. ROLE IN DEFENSE MESCHANISM
1. color
2. Volume 5 L
3. pH 7.4
4. Specific gravity
5. Viscosity
BLOOD CELLS
1. RED BLOOD CELLS OR ERYTHROCYTE
2. WHITE BLOOD CELLS OR LEUKOCYTES
3. PLATELETS OR THROMOCYTES
PLASMA
Plasma is a straw colored clear liquid part of blood. It
contains 91%-92% of water
and 8%-9% of solids.
SERUM
Serum is the clear straw colored clear liquid fluid that oozes
from blood clot. When the blood is shed or collected in a container it
clots. In fibrinogen is converted into fibrin and blood cells are trapped in
this fibrin forming the blood clot. After about 45 minutes serum oozes out of
the blood clot.
SERUM = PLASMA - FIBRINOGEN
1. NUTRITIVE FUNCTION
2. RESPIRATORY FUNCTION
3. EXCRETORY FUNCTION
4. TRANSPORT OF MORMONES AND ENZYMES
5. REGULATION OF WATER BALANCE
6. REGULATION OF ACID BASE BALANCE
7. REGULATION OF BODY TEMPERATURE
8. STORAGE FUNCTION
9. DEFENSIVE FUNCTION
PLASMA PROTEINS
Plasma proteins are
1. Serum albumin
2. Serum globulin
3. Fibrinogen
NORMAL VALUE OF THE PLASMA
PROTEINS
1. Total proteins : 7.3g/dL
2. Serum albumin : 4.7g/dL
3. Serum globulin : 2.3g/dL
4. Fibrinogen : 0.3g/dL
2. Serum albumin : 4.7g/dL
3. Serum globulin : 2.3g/dL
4. Fibrinogen : 0.3g/dL
METHODS
1. PRECIPITATION METHOD
2. SALTING OUT METHOD
3. ELECTROPHORESIS METHOD
4. COHNS FRACTIONAL PRECIPITATION METHOD
5. ULTRACENTRIFUGATION METHOD
6.GEL FILTRATION CHROMATOGRAPHY
7. IMMUNOELECTROPHORETIC METHOD
FUNCTIONS OF PLASMA PROTEINS
1. ROLE IN COAGULATION OF BLOOD
2. ROLE IN DEFENCE MECHANISM OF BODY
3. ROLE IN TRANSPORT MECHANISM
4. ROLE IN MAINTENANCE OF OSMOTIC PRESSURE IN BLOOD
5. ROLE IN REGULATION OF ACID BASE BALANCE
6. ROLE IN VISCOSITY OF BLOOD
7. ROLE IN ERYTHROCYTE SEDIMENTATION RATE
8. ROLE IN SUSPENSION STABILITY OF RED BLOOD CELLS
9. ROLE IN PRODUCTION OF TREPHONE SUBSTANCES
10. ROLE AS RESERVE PROTEINS
RED BLOOD CELLS
Red blood cells are the non nucleated formed elements in the
blood. Red blood cells are also known as erythrocytes. Red colour
of the red blood cells is due to the presence of the coloring pigment called
hemoglobin.
NORMAL VALUE
RBC count ranges between 4 and 5.5 million/cu mm of blood. In
adult males, it is 5 million/cu mm and in adult females it is 4.5 million/ cu mm
.
The RBC are disk shaped and biconcave central portion is thinner
and periphery is thicker. The biconcave contour of RBCs has some
mechanical and functional advantages.
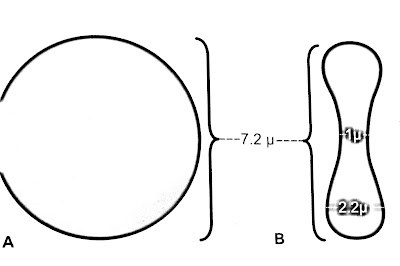 |
| DIMENSION OF RBC |
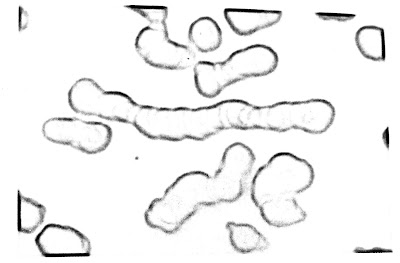 |
| ROULEAU FPRMATION |
PROPERTIES OF RED BLOOD CELLS
1. ROULEAUX FORMATION
2. SPECIFIC GRAVITY
3. PACKED CELL VOLUME
4. SUSPENSION STABILITY
1.
Transport
of oxygen from the lungs to the tissue
3. Buffering action in blood
VARIATIONS IN NUMBER OF RED BLOOD CELLS
A. Increase in RBC count
1. Age
2. Sex
3. High altitude
4. Muscular exercise
5. Emotional conditions
6. Increased environmental
temperature
7. After meals
B. Decrease in RBC count
1. High barometric pressures
2. During sleep
3. Pregnancy
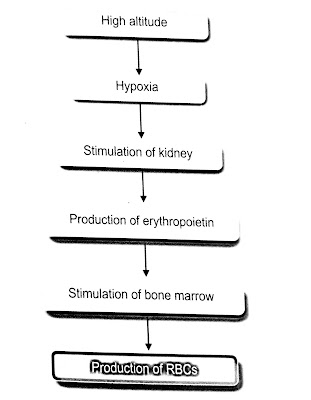 |
| PHYSIOLOGICAL POLYCYTHEMIA IN HIGH |
 |
| PHYSIOLOGICAL POLYCYTHEMIA IN EMOTIONAL CONDITIONS EXERCISE |
It is a process of origin or formation of erythrocytes. It starts
in the third week of intra uterine life and remains continues as long as the
person is alive.
Definition
Erythropoiesis is the process of the origin development and
maturation of erythrocytes. Hemopoiesis or hematopoiesis is the process of
origin development and maturation of all the blood cells.
SITE OF ERYTHROPOISIS
IN FETAL LIFE
In fetal life the erythropoiesis occurs in 3 stages
1. Mesoblastic stage
During the firt 2 months of
intrauterine life the RBCs are produced from mesenchyme of yolk sac.
From third month of intrauterine life liver is the main organ that
produces RBCs. Spleen and lymphoid organs are also involved in erythropoiesis.
3. Myeloid stage
During the last 3 months of
intrauterine life the RBCs are produced from red bone marrow and liver.
STAGES OF ERYTHROPOIESIS
1. Proerythroblast
2. Early Normoblast
3. Intermediate Normoblast
4. Late Normoblast
5. Reticulocyte
6. Matured Erythrocyte
GENERAL FACTORS
1. Erythropoietin
Most important general factor for erythropoiesis is the hormone
called eruthropoietin . It is also called hemopoitin or erythrocyte
stimulating factor.
Hypoxia is the stimulant for
the secretion of erythropoietin.
2. Throxine
Being a general metabolic hormone thyroxine accelerates the
process of erythropoiesis at many levels. So hyperthyroidism and polycythemia
are common.
Hemopoietic growth factors or growth inducers are the interleukins
and stem cell factor . Generally these factors induce the proliferetion of
PHSCs. Interleukins are glycoproteins, which belong to the cytokines family.
4. Vitamins
Some vitamins are also necessary for the process of
erythropoiesis. Deficiency of these vitamins cause anemia associated with other
disorders.
Vitamins necessary for
erythropoisis
A. Vitamin B
B. Vitamin C
C. Vitamin D
D. Vitamin E
MATURATION FACTORS
1. Vitamin B12
Vitamin B12 is called extrinsic factor since it is obtained mostly
from diet. Vitamins B12 is stored mostly in liver and in small quantity in
muscle.
2. Intrinsic Factor of Castle
Intrinsic factor of castle is produced in gastric mucosa by the
parietal cells of the gastric gland.
Folic acid os also essential for maturation. It is required for
the synthesis of DNA.
WHITE BLOOD CELLS
Definition
WBC are pigmented cells of short life span which are extra
vascular in origin. These are rich in nucleoprotein and also contain
cholesterol and glycogen.
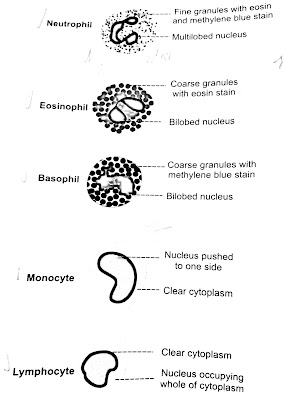
1. NEUTROPHILS
Neutrophils which are also known as polymorphs have fine or small
granules in the cytoplasm. The granules take acidic and basic
stains.
When stained with LEISHMANS STAIN the granules appears violet in color.
When stained with LEISHMANS STAIN the granules appears violet in color.
2. EOSINOPHILS
Eosinophils have coarse granules in the cytoplasm which stain pink
or red with eosin.
3. BASOPHILS
Basophiles also have coarse granules in the cytoplasm. The
granules stain purple blue with methylene blue.
4. MONOCYTES
Monocytes are the largest leukocytes with diameter 14 to 18
. The cytoplasm is clear without granules. Nucleus is round oval and
horseshoe shaped bean shaped or kidney shaped.
Like monocytes the lymphocytes also do not have granules in the
cytoplasm.
VARIATIONS IN WHITE BLOOD CELL COUNT
1. Leukocytosis
2. Leukopenia
3. Granulocytosis
4. Granulocytopenia
5. Agranulocytosis


0 comments:
Post a Comment